Scoliosis Awareness Month: What to Know About This Disease
June is Scoliosis Awareness Month. The goal of this is to to educate, learn early detection and bring awareness about this disease.
From walking to breathing, the structural stability of our spine plays a key role. This is why severe scoliosis is debilitating if left untreated, and why untreated scoliosis can get worse as time passes and we put our body under exceeding amounts of stress. To understand scoliosis and the challenges it poses, it’s important to be aware of why and how the spine is important.
The condition of the spine determines our ability to move, stand, lie down, and generally be alive. Not only is it a physical pillar for our entire musculature, but the spine features the spinal cord, the only part of our primary nervous system/central nervous system not located exclusively in the brain. Damage to the spinal cord can be life-threatening, and can lead to paralysis, pain, and other forms of disability, severely affecting motor control.
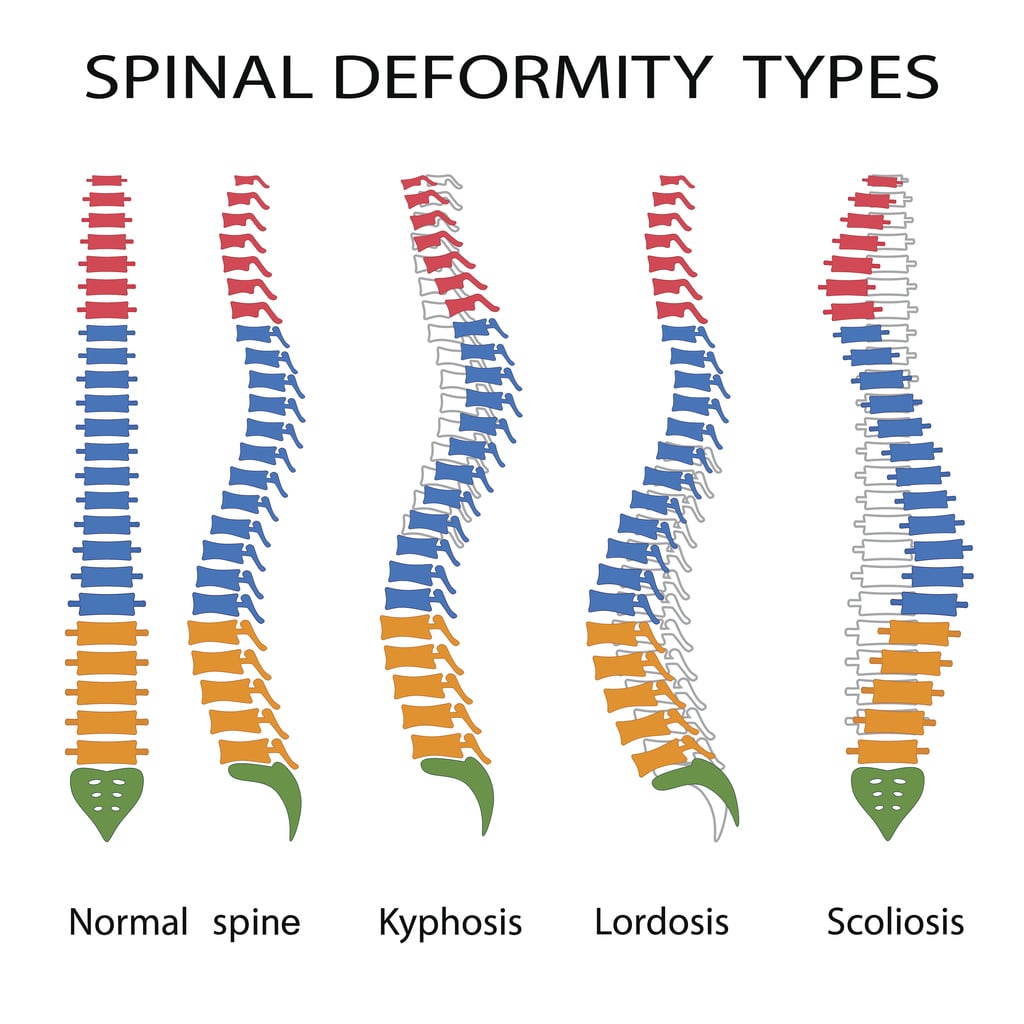
In normal cases, the spine possesses a natural curve as it begins from the brainstem, all the way down to the tailbone. From top to bottom, it’s divided into six regions: the cervical (neck), thoracic (upper back), lumbar (lower back), sacrum (behind the glutes), and the coccyx (the tailbone). Curving almost like an S from a lateral view, the spine ideally maintains a straight line throughout the body when a person faces you.
Surrounding the spine are a series of muscles and bones critical for movement and survival. The placement of the rib cage is incredibly reliant on the angle of the spine, and in turn, determines how your organs grow and how your lungs expand during breathing. As we walk, lift objects, bend over, and lie down, different loads are exerted onto our bodies by gravitational forces and additional resistance, putting the spine under compression and shearing forces.
Lifting a box off the ground with your back, for example, will cause your vertebrae to potentially shift apart, thus requiring a straight spine and a strong back for support. Pushing something overhead, on the other hand, can place additional stress in a straight line down the center of your body (and onto your spine), compressing your vertebrae together.
So, for us to perform basic physical tasks – and even just walk and lie down without pain – our spine must be in a natural neutral position. Our spine curves naturally from a lateral view and straight from an anterior view.
But what happens if the spine is curved abnormally?
This Scoliosis Awareness Month, Comprehensive Pain Management Center strives to teach about this debilitating disease; the symptoms, causes, and treatments of scoliosis.
What is Scoliosis?
To expand scoliosis awareness, we’ll first explore what scoliosis is.
When viewed from the front, scoliosis presents as a sideways curvature of the spine, most often in the thoracic portion of the spine. Its symptoms often begin in adolescence and become more pronounced towards the end of puberty and in adulthood, and the curvature can rank anywhere from mild to very severe.
Mild scoliosis may lead to muscular imbalances, certain mobility issues and mild back pain, while severe scoliosis can lead to difficulty breathing, damage to the organs in and around the ribcage (especially the heart and lungs), and greater risk of injury through shearing forces applied to the spine.
Scoliosis is not the excessive curvature of the spine’s natural curves – these are usually symptoms of other spine-related issues, caused by injury, disease/infections, muscular weakness, or imbalance, and are described as kyphosis (a rounded upper back, also known as a hunchback) and lordosis (excessive curvature in the lower back, causing an anterior pelvic tilt).
While a person can present with both scoliosis and lordosis/kyphosis, these are separate spine issues. Each of them, however, come with complications related to back pain and quality of life.
Scoliosis Awareness: Identifying the Disease
Scoliosis awareness of symptoms are visually obvious in severe cases, appearing as significant unevenness in the hips and shoulders, and a tilt of the upper or lower back towards one side.
In mild cases, scoliosis can still present as unevenness in the shoulders, best measured by seeing if the collarbone aligns correctly. A proper diagnosis requires a thorough checkup by a medical professional.
While there is such a thing as the ideal human spine, it’s important to remember that human bodies are imperfect.
Imbalances are natural, and it’s not uncommon to have a slight sideways curvature in the spine, especially as a result of years of imbalanced loading, such as holding more weight on one side than the other in the form of a suitcase or heavy school bag.
For the sideways curvature of the spine to be considered scoliosis – a diagnosable condition in need of some form of treatment – most professionals look for a curve of at least >10 or >15 degrees. Anything below is unlikely to cause any issues for that person down the road.
What Causes Scoliosis?
While expanding scoliosis awareness, it’s important to learn what causes this debilitating disease.
However, the causes of most cases of scoliosis are virtually unknown. While we understand that genes have some role to play in how a person’s spine develops, it’s difficult to pinpoint the exact cause in most cases of scoliosis.
These are idiopathic scoliosis. In other, rarer cases, it may be the result of a neuromuscular disorder (neuromuscular scoliosis), birth defects (congenital scoliosis), or severe injury to the spine and surrounding tissue.
Another form that typically occurs with old age is degenerative scoliosis, which occurs because of atrophy of musculature around the spine.
Mild scoliosis can also be functional or nonstructural scoliosis, a temporary change in spinal curvature usually due to excessive force on one side of the body, another structural issue altogether (a shorter leg, for example), or musculoskeletal conditions causing muscle spasms and involuntary contraction.
Postural scoliosis is also a form of nonstructural or functional scoliosis. This can reverse itself without the need for any invasive treatment.
Healing Your Spine
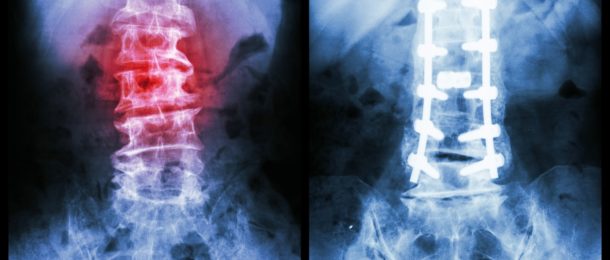
The goal behind scoliosis awareness and treatment is diminishing the sideways curvature of the spine to the point where the patient no longer presents with back pain or organ damage because of their condition.
One way to further affect the effect scoliosis has on their bodies is through physical therapy and exercise. A pain management specialist will be able to improve your scoliosis awareness, and in turn create a pain strategy to effectively reduce your pain.
While scoliosis can limit a person’s mobility, it does not have to limit their strength or quality of life.
An extreme example is Lamar Gant, a renown American powerlifter with significant idiopathic scoliosis, and world records in the conventional deadlift, pulling around five times his own bodyweight off the floor.
Other examples of notable athletes with scoliosis include Usain Bolt and James Blake.
While scoliosis does present challenges to anyone pursuing athletic ability, the condition does not deny you your dreams. Several treatments today can greatly reduce the curvature of the spine, including invasive methods like surgery, and less invasive, effective methods such as physical therapy, and limited time spent in a spinal brace.
By gradually and consistently pushing the spine into a more natural position and greatly strengthening the muscles around the spine – particularly the erectors and trapezius – anyone with scoliosis can make great progress. Therapy to fix muscular imbalances because of spinal curvature can also mitigate back pain and reduce muscle spasms.
Scoliosis is a chronic disease, which means it does get worse and comes back if not regularly counteracted and treated. However, regular exercise and frequent checkups can drastically improve your quality of life, and even make you pain-free.
Contact your pain management center today to learn more about scoliosis awareness, and how you can treat this disease.
Arthritis Awareness Month: Different Types of Arthritis to Know
May is Arthritis Awareness Month, and we are here to support over 50 million Americans struggling with different types of arthritis, with patients of all ages and backgrounds.
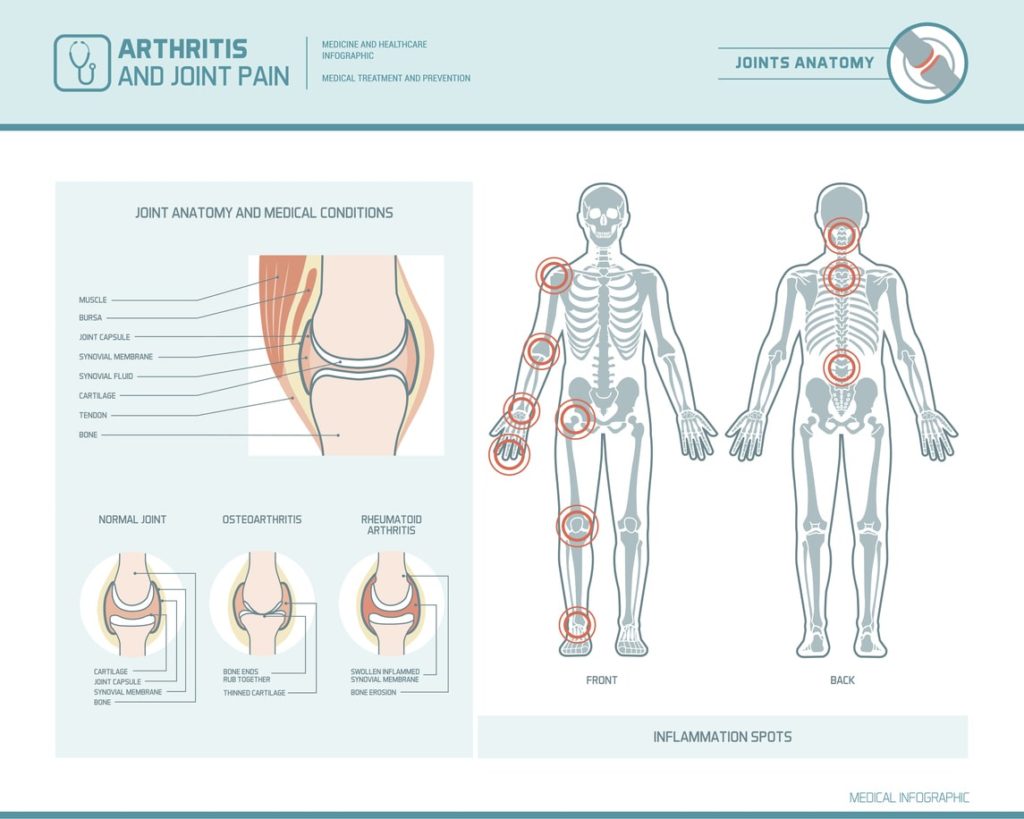
An inflammatory disease, arthritis is characterized by inflammation and pain in the joints. Common symptoms include joint stiffness, swelling, and feverishness.
Different types of arthritis can range from presenting mild pain to becoming a debilitating musculoskeletal disease, and while it mostly affects people aged 65 and older, it is also present in some form in children, teens, and young adults.
Why Participate in Arthritis Awareness Month?
As a pain management center, we focus heavily on arthritis, and how it affects the lives of our patients.
Arthritis is an extremely common, yet misunderstood disease. This Arthritis Awareness Month, we will show support to our clients, and everyone suffering from arthritis.
This Arthritis Awareness Month, our goal is improve knowledge of this disease by discussing the different types of arthritis.
Because of the many different types of arthritis, it can be difficult to receive the right treatment that works for you. Our goal is to help explore the different types of arthritis, their symptoms, and how to ease each type of pain.
To understand arthritis, it is important to understand its sources – and how it can manifest. More than just a symptom of old age, arthritis is something nearly 400 million people struggle with worldwide. It’s often a source of such pain that it can drastically affect the way people live and work.
In fact, a report by the CDC notes that a third of arthritis patients in the US report that the disease limits their livelihood and leisure.
What Are the Different Types of Arthritis?
While it is a widespread condition, arthritis is tough to understand. Misconceptions muddy the public understanding of what this disease is, and how it occurs.
By definition, arthritis is any condition involving the inflammation of the joints. In general, a breakdown of the body causes arthritis, either in the form of aged or overused joint tissue and cartilage, or through an immune reaction.
There are many different types of arthritis, and sources of arthritis vary and depend from condition to condition.
Below, we’ll explore the 4 different types of arthritis that are most common.
4 Common Types of Arthritis
Arthritis, despite the simple definition, comes in over a hundred different forms.
We will go over the different types of arthritis that are most common, and describe their origins, symptoms, and possible treatment options.
- Osteoarthritis
- Fibromyalgia
- Rheumatoid Arthritis
- Psoriatic Arthritis
We will go into detail about the different types of arthritis below.
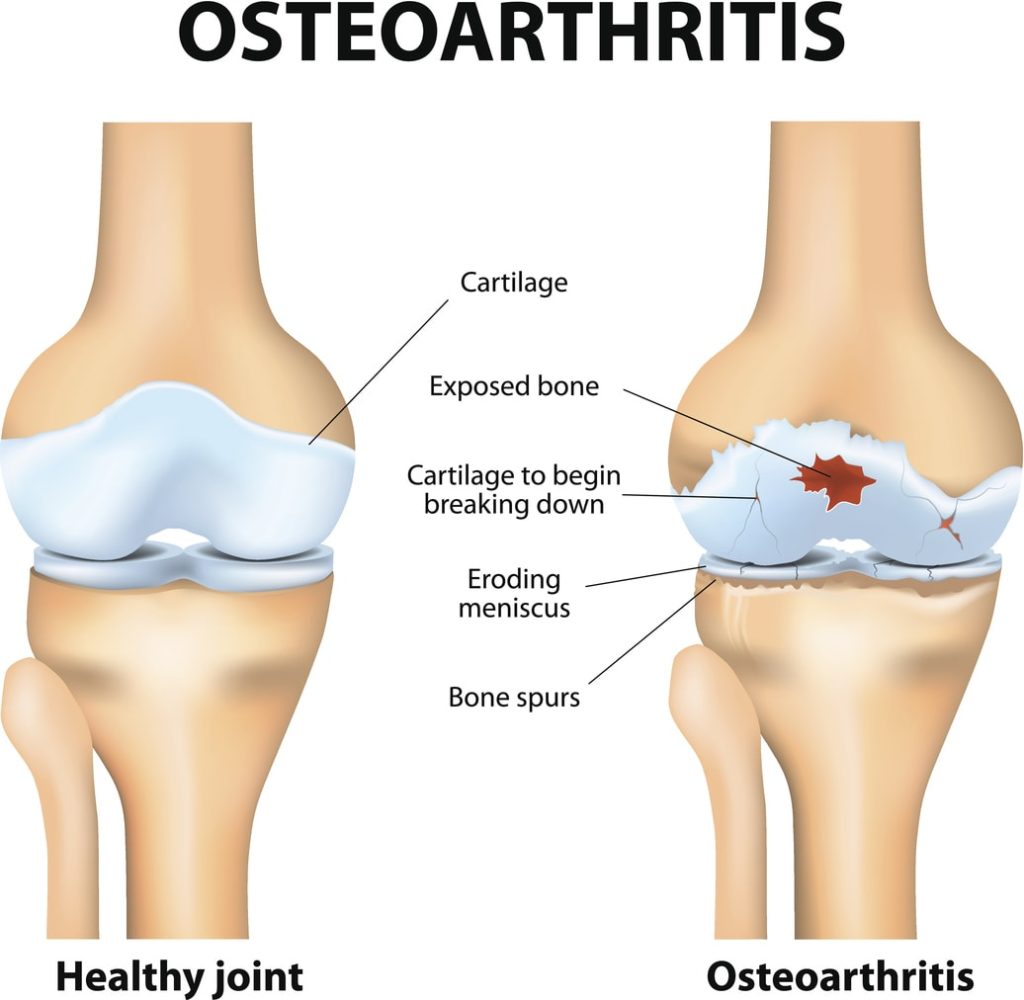
1. Osteoarthritis
Known as the most common form of arthritis, osteoarthritis is centered in the joints and involves the deterioration of joint cartilage.
As we walk, run and jump, the protective ends of our bones wear down through constant impact. This affects our joints the most, as they receive and process the most force in any given movement. However, osteoarthritis can also affect the hips, and spine.
Due to the nature of wear and tear, it is most common in people 65 or older. However, genetics or lifestyle choices can speed up the rate at which a person’s cartilage wears down. This then accelerates the symptoms. These primarily include pain, swelling and tenderness around areas where the cartilage is wearing down.
Treatment of Osteoarthritis
Treatment involves the prevention of further deterioration, and the regeneration of cartilage, as well as pain management. While exercising might be counter-intuitively seen as a cause of cartilage wear down, strengthening the muscles and tendons around the bones can take a lot of stress off the joints, thus decreasing the rate at which your osteoarthritis progresses.
Exercise can also help you better manage pain, both through a release of endorphins and by strengthening the body.
Weight loss is also an option. Obesity increases the risk of arthritis by placing more pressure on the joints. Likewise, an unhealthy lifestyle options can lead to weaker bones and cartilage due to poor nutrition.
Adopting better eating and movement habits will reduce pain, slow the arthritis, and improve your quality of life. Be careful not to overdo it. Exercise as appropriate for your body’s current condition and strength. At times, simply walking more often can produce a positive change for your symptoms. Over time, you can move on to more strenuous exercise, as per your doctor’s recommendation.
2. Fibromyalgia
Classically, arthritis is a joint-related disease, but fibromyalgia is connected to arthritis through widespread pain not only in the joints, but throughout the musculoskeletal system.
Plagued by an incomplete understanding of the disease, the medical community still has trouble identifying concrete causes for fibromyalgia. While it is centered in the nervous system, it is known as a specific set of symptoms, rather than a single disease centered on a known source.
Fibromyalgia affects nearly 4 million Americans, most of them women. Its connection to arthritis is difficult to understand. However, people struggling with forms of arthritis – including rheumatoid arthritis and lupus – are at a greater risk of developing fibromyalgia as well.
Treatment of Fibromyalgia
Suspected causes or factors in the development of fibromyalgia include an extended exposure to physical and emotional pain, particularly trauma. Hormonal changes or an infectious illness also are a suspect of cause as well. Another possible link is poor gut health, from bacterial overgrowth to other problems sourced in a person’s gut flora.
Treatment for fibromyalgia largely involves pain management. Until a person’s individual cause for pain is identified, their treatment lessens the effects the disease has on their life.
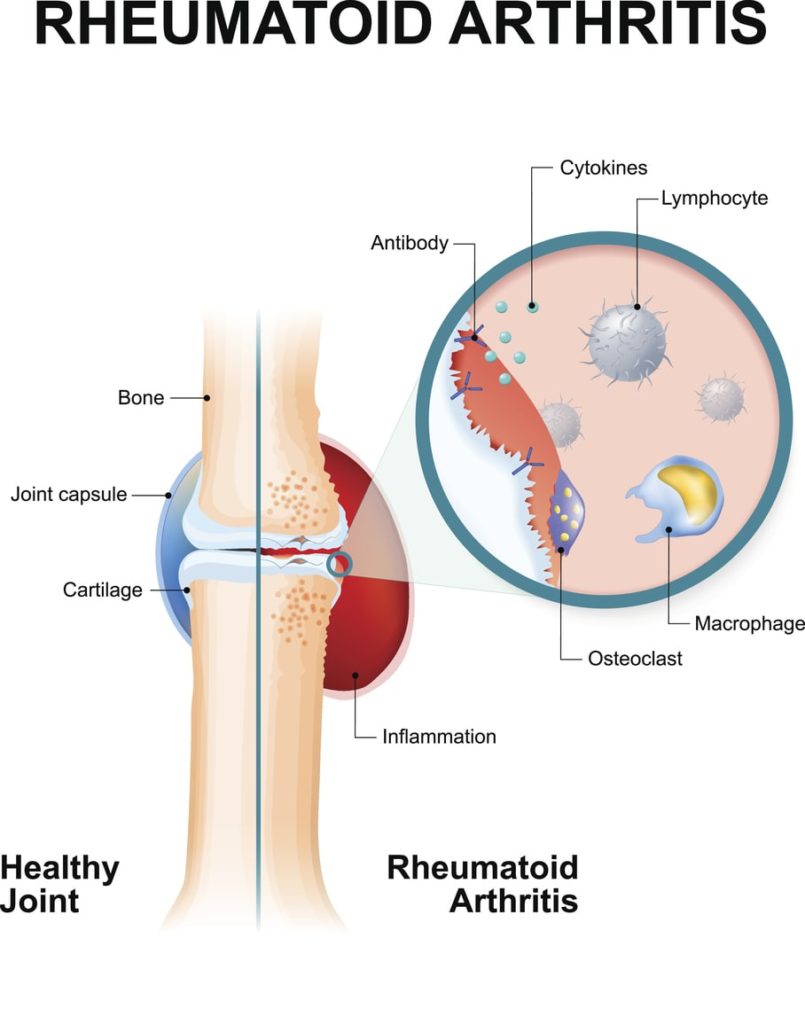
3. Rheumatoid Arthritis
Much like osteoarthritis, rheumatoid arthritis affects most joints.
But rather than wear-and-tear, rheumatoid arthritis is defined by the inflammation of the lining around joints due to an autoimmune reaction.
Your immune system begins attacking your joints, skin, blood vessels, and even other organs like your heart and lungs.
Long-term rheumatoid arthritis, if left untreated, can be debilitating and can cause disability.
Treatment of Rheumatoid Arthritis
However, several treatments exist to combat the symptoms, and stop the disease from progressing.
Non-addictive painkillers, antirheumatic drugs, and medicine that specifically targets inflammation can help, and can help to combat RA.
4. Psoriatic Arthritis
Psoriasis is a chronic skin condition that essentially accelerates the rate at which your skin cells age, causing a fast buildup of dead and dying skin. It is commonly identified through red patches and itchy scales and is caused by an autoimmune reaction that erroneously forces your skin cells to grow much too quickly.
As part of psoriasis, you can develop joint pain, stiffness, and inflammation.
Treatment of Psoriatic Arthritis
Out of the different types of arthritis, this one is chronic, reoccurring with the condition itself. While a permanent cure does not exist, treatment focuses on forcing the condition into remission.
Other diseases tied to arthritis include gout and lupus, as well as a long list of more complex or specific disorders and conditions. Each one requires personalized treatment, involving medical, physical, and mental treatment options.
Tackling Pain
As a disease primarily centered around pain, pain management plays a critical role in fighting arthritis. While pharmaceutical tools exist to help combat acute pain, prescription painkillers are too much of a risk, for too little reward. Their potential for addiction and abuse is high, while their effectiveness fades with time, making them an impotent solution for chronic pain.
Instead, comprehensive pain management through a reputable clinic near you can offer a long-term solution for pain. Your specialist will help with physical therapy, opioid alternatives, talk therapy, mind-body techniques, alternative medicine and more.
Each case of arthritis is unique. Professionals must consider a person’s symptoms in relation to their lifestyles, circumstances, and possibilities to consider treatment options, and devise an effective plan for a better quality of life.
Understanding your own disease can go a long way towards combating it. However, by giving you a bigger picture of why you’re in pain, how your body is struggling, and what you have to do in order to follow your physician’s or specialist’s instructions and improve your symptoms.
As in any case, do not attempt any treatments yourself or begin applying exercise and drastic diet changes to yourself without first consulting a medical professional, and getting a full checkup. It’s important to know how your pain began and why you’re experiencing it before taking measures to treat it.
This Arthritis Awareness Month, take some time to learn the different types of arthritis; their symptoms and treatment options. Talk to your pain management specialist to create a personalized plan to reduce pain and lead you to a life of happiness.
How Is Cognitive Dysfunction Linked to Pain?

It is no secret that we cannot think clearly when we are in pain. The brain reacts in a certain way when experiencing pain – pain is not only a message from the body to the brain, but it kicks certain emotions into autopilot, while actively hindering you from thinking straight or performing complex tasks. When pain is at its worst, your thoughts are chaotic. You experience what is basically best described as cognitive dysfunction – also known as “brain fog”.
What is Cognitive Dysfunction?
Cognitive dysfunction is a condition from a myriad of diseases, environmental factors, and genetic conditions. It is a decline in a person’s cognitive abilities, or a loss of intellectual capability, even if only temporary.
As “brain fog” implies, cognitive dysfunction is diagnosed by a marked decrease in cognitive ability, especially versus the norm. When testing for cognitive deficiency in patients with chronic pain, researchers created a control group and a group of patients, all with similar backgrounds in terms of education, and tested their cognitive abilities through IQ tests, memory tests, and more.
Unlike certain diseases that target a specific part of the brain, cognitive dysfunction is a symptom of a condition that blanketly decreases a person’s ability to think. Pain is one such condition.
What is Pain?
Pain is all about thinking – after all, it is all in your head. But that does not make it any less real. In fact, pain connecting to your brain means it is about as real as something can be. Understanding pain can give you a clear insight into why pain is commonly linked with cognitive dysfunction. It can even give some people clues as to how to better regulate their pain.
When the brain experiences pain, it is typically because certain brain cells – called nociceptors – are transmitting a “noxious” feeling, noxious basically meaning bad. This is due to a series of things, things that make us feel pain as a basic defensive response.
Anything from being burnt, experiencing spontaneous muscle cramping, receiving sharp or blunt trauma, or even an emotional blow on par with a breakup or disinheritance can be enough to cause your nociceptors to make you experience pain.
This is a defensive mechanism – a strong reminder from our brain to not do that again, to preserve our life.
Why Chronic Pain is No Ordinary Pain
Pain is experienced subjectively and can only be described in a person’s own words. Factors such as mood and even culture affect this experience as well.
Everyone has experienced pain, from mild discomfort to severe distress. Yet severe pain will always trigger a person’s survival instincts, including their fight-or-flight response. It is not uncommon for pain to send someone into a fit of rage or send a dosage of adrenaline through their system. As such, it is normal to assume that when you are experiencing pain, you cannot think properly.
Yet different from this acute pain, chronic pain is any pain that lasts longer than 12 weeks, or approximately three months. Chronic pain due to a wide array of diseases, both physical and mental.
It can be attributed to anything from surgery and injury, to genes and brain disorders. A professional creates a diagnosis, after considering all the factors and circumstances of your case.
How Chronic Pain Is Different
Regardless of the cause, however, chronic pain is unique in the fact that it simply does not go away like acute pain does. When you receive a blow to the head, your head will hurt for a while. This is acute pain. The area around the damaged tissue will be tender and sensitive, as this is part of the body’s defense mechanism – to prevent anyone from further damaging that area. Yet after a while, the pain passes.
If you are the subject of a specific pain repeatedly, you develop a tolerance to it. This is what stretching is. Studies show that stretching does not impose a physical change to the body’s tendons or musculature. Rather, it simply affects the brain’s pain tolerance and stretch tolerance. This temporarily increases your ability to stretch beyond normal limitations due to repeated stretching.
Chronic pain, however, is different. People with chronic pain experience a change in the way the spine, nerves, and brain process pain. Whatever the cause of their condition, it has effectively warped the way they experience pain. This means that it potentially does not get “easier” with time, unless treated accordingly. In some cases – such as fibromyalgia – it can get actively worse with time.
Exploring the Cognitive Consequences of Chronic Pain
Living with chronic pain introduces several challenges that affect a person’s ability to think, leading to cognitive dysfunction. For one, the pain itself can present difficulties, acting as a frequent source of distraction and irritability. There is also the correlation between chronic pain, and negative thinking, as well as mental conditions such as anxiety and depression.
These conditions, in turn, actively worsen the effects of chronic pain by amplifying the experience. Research has also shown that, on top of pain, episodes of depression frequently limit a patient’s cognitive abilities, keeping them from thinking straight or performing well on tests of verbal and spatial memory, attention, and executive functioning.
Several studies show that chronic pain is not only a factor in causing brain fog within individuals, but it can amplify existing factors that attribute to cognitive decline, including mood and age.
Young adults with chronic pain experienced a much lower degree of cognitive dysfunction versus aging patients, stressing the importance of adequate and effective treatment to lessen the impact of chronic pain on a patient’s quality of life.
Improving Cognition in Patients with Chronic Pain
Chronic pain directly affects cognitive ability, regardless of a person’s perception of said pain culturally. For example, certain cultures are less likely to speak about pain or address it with less importance than Western cultures. They also report a higher pain tolerance. Despite this, studies performed on both Western adults and Middle Eastern adults finds similar cognitive deficiencies.
That is not to say that mindset does not affect cognition. Cognitive rehabilitation is possible for patients with chronic pain, but it must concern itself with addressing the pain and the patient’s mood and emotional state, to alleviate the brain fog caused by the undue stress of chronic pain.
Stress and emotional pain – from shame or anger due to certain limitations imposed by the pain, to depression and anxiety from feeling isolated – can amplify the effects chronic pain has on a person’s intellect.
Addressing these issues, as well as sleep disturbance and fatigue, is of great importance. If you are experiencing constant cognitive dysfunction and emotional distress, seek professional help. Only after a thorough assessment of your condition and circumstances can professionals recommend specific treatments.
10 Surprising Facts About Integrated Pain Management

Integrated pain management is vital to millions of Americans. From post-surgery or postpartum care, to chronic pain caused by injuries or diseases, a crucial part of delivering expedient and quality medical services to the American people includes managing every patient’s pain in a safe and effective manner.
Despite its importance, pain management is a relatively obscure branch of medicine for many. Here are a few facts about most pain management clinics and integrated pain management techniques that may surprise you.
1. We Consider Every Effective Method
Integrated pain management clinics often include a long list of treatments in their repertoire for effective pain management – as long as these treatments have a proven history of usefulness, and the clinic employs the experts needed to help administer these treatments. Pain management has grown exponentially since it first became a major aspect of medicine, and countless techniques have shown to be of some use under certain circumstances.
However, just because many clinics cover both traditional as well as conventional (or Western) and alternative medicine, does not mean that every treatment is useful in every occasion. Most reputable clinics make it a point to create and tailor a treatment plan that includes only the treatments most likely to work for a specific patient.
2. Many Clinics Shy Away from Opioids
It is no secret that the US has an opioid problem. However, the medical community has begun to take steps to address it. Increased regulation as well as differing attitudes among medical professionals is having an impact on the crisis – while many people still source their prescription medication illegally, or use stashes from years ago, some pain management specialists are shying away from opioids as anything other than post-surgery care for acute pain, or in hospice.
Integrated pain management sometimes means finding a way to live life with the pain, and to focus on the healing rather than masking it with numbness. In other cases, alternative medicines combat the effects of pain. Experimental medicines are still being developed to completely replace opioids, providing relief without addictiveness.
3. Doctors Agree that Lifestyle Changes Are Vital
There is a common misconception that professionals in the medical field are out only for the money, and do not take into consideration the amount of healing and relief the body can experience through lifestyle changes. This is not true. Most reputable medical professionals will agree that making changes to your lifestyle – especially with low-impact exercises and anti-inflammatory foods – is important for long-term pain management and longevity.
Doctors advise this often, but also know that such advice can fall on deaf ears. Pain management is about more than relying on one path. It is about finding a course of action that works for the patient, even if it requires the use of several different techniques. As such, a pain management specialist will look towards other alternative methods of pain relief, as well, including non-opioid medication, non-invasive treatment, acupuncture, and more.
4. The Mind is Important
Mindfulness training and cognitive behavioral therapy are just two of several common mental health treatments that are finding application and usefulness in the world of integrated pain management. Research has shown that not only is pain affected by a person’s mindset and outlook, but acute mental distress can drastically change the way someone feels and perceives their body. This can cause greater pain than ever.
Through psychotherapy and mental training exercises, an integrative pain management clinic can teach patients how to take charge of their mindset and use their perspective to combat their pain.
5. Chronic Pain Is Not Always Permanent
Chronic pain describes a condition wherein a patient experiences pain lasting for more than 12 weeks. However, despite the fact that chronic pain implies a long-lasting pain caused by major trauma, it is not always permanent. Pain management does not entail having to deal with said pain for the rest of your life.
A big part of integrated pain management is ensuring that the underlying cause of chronic pain is pin-pointed and identified. Some causes, such as fibromyalgia, do not have a straightforward cure yet. Others, such as a long-standing injury or certain nerve-related pain may ease through the right physical therapy and treatment approach. Pain management can also be about helping patients deal with the naturally-occurring pain of the healing process after a major surgery or accident.
6. Opioids Don’t Necessarily Treat Chronic Pain
Opioids are incredibly powerful analgesics – but the nature of the drug means continuous use wears out its effects, as the body begins to acclimate to the opioid. This makes opioids less effective in managing pain over a long-term period.
Adding onto that their risk of addiction means they do not make for a reliable or very useful tool in integrative pain management for most types of pain. There are cases when opioids are still available within reason – such as after a major traumatic wound, in emergency care, or after an invasive surgery. Some cases of end-of-life pain also use opioids. But for the patient looking for a way to deal with their chronic pain, opioids are not a good solution, even if the risk of addiction is set aside.
7. Pain Management is For All Ages
Integrative pain management is not only for people in their final stages of life – accidents, diseases, disorders, and other circumstances can create the conditions for excruciating and long-lasting pain, from birth to death. Integrative pain management takes every aspect of a patient’s life into account when formulating an effective treatment plan, including their age. Therefore, pain management professionals are capable of helping patients of all ages.
8. Integrated Pain Management Clinics Care About Their Patients
Much like with the idea of doctors focusing on profitable treatments over effective ones, reputable pain management clinics are tasked with prioritizing patient safety and work with non-profit, voluntary organizations like the Leapfrog Group to ensure a high standard of patient care, quality, and customer safety. The medical community is not just driven by profit, but by a system of reputation. Low-quality medical care that does not stay true to the medical oath is not acceptable.
9. Anxiety and Depression Aggravates Pain
A patient’s mental status can affect how they deal with pain. However, nothing upsets chronic pain more than a constant state of anxiety and/or depression. These two conditions can disrupt a person’s quality of life. It cuts into their ability to manage their pain, and makes them lose hope for the future. It does this by convincing them that the pain will get worse, or that their condition will never have a cure.
An integrated pain management clinic tackles the mental as well as the physical aspects of a patient’s health. This helps them create the best possible environment to tackle their pain.
10. Pain Management Can Help You Keep a Job
Chronic pain does not immediately equal disability, nor does a temporary disability mean you will not be able to work again. Many patients worry about their ability to continue contributing after their condition has become aggravated. However, pain management also includes helping you find a way to do the things you need to do while minimizing your pain as well.
Yes, chronic pain and certain conditions will limit your ability to work – but it need not eliminate it.
Hopefully these ten facts about integrated pain management will shed some light into this field and help you to find the best pain management clinic for you.
How A Pain Management Specialist Can Help You

Pain is a natural part of life, but for many Americans, its role daily becomes unmanageable and consistently excruciating. From illnesses like fibromyalgia, to injury-related long-term nerve damage, there are many ways for pain to become a chronic element in a person’s life, and beyond the usual avenues of prevention and cure, many Americans turn to a pain management specialist to help with pain management.
A pain management specialist exists to help patients cope with chronic pain and all its facets, relieving pain through physical and mental therapy, and responsible medication.
4 Ways a Pain Management Specialist Can Help
Professionals today understand the nature of pain better than ever before. We can help patients find joy and comfort in living life again. These pain doctors have a wide array of knowledge, and can help assist you with multiple types of pain. These include:
- Chronic Pain
- Cancer Pain
- Joint Pain
- Pregnancy Pain
Depending on the type of pain you suffer from, your pain management plan will vary. Your pain doctor will help you to create such a plan after initial meetings.
Here are a few examples of what a pain management specialist can offer you.
Providing Help with Chronic Pain
Chronic pain sets itself apart from acute pain by duration. When a painful sensation regularly reoccurs, or lingers for more than 3 months (12 weeks), then it is a chronic pain. Causes for chronic pain are typically nerve-related. This includes nerve trauma, to a pinched nerve, an oversight in surgery, accumulated damage from years of injuries and recoveries, arthritis, infections, certain illnesses and more.
Because of the many causes of chronic pain, and because of the countless forms it can take – from a constant, dull headache, to stiff joints, or a sharp pinch in your wrist – every case and complaint of chronic pain requires an intense investigation, and personalized care.
Trained pain management specialists work with physicians and experts to determine the cause of your pain. Together, they focus on relieving it in the best and least invasive manner.
While pain management is known for the use of strong medication like opiates (including morphine, and less potent prescription drugs), these substances can be dangerous due to their addictiveness and are highly regulated, and not lightly prescribed. Instead, several alternatives are offered, including major lifestyle changes, changes in diet and exercise, and alternative treatments such as acupuncture and hypnotherapy.
Help You Fight Cancer-Related Pain
Cancer can be painful – not just emotionally, but physically. The deterioration of organ tissue, alongside the unpleasantness that accompanies tumor growth pushing against nerves and bones, is the cause for much pain over the course of cancer treatment, both acute and chronic. Chemotherapy, while often necessary for treatment, can also come with serious side-effects that deteriorate quality of life and introduce pain in the form of burning sensations and more.
A pain management specialist can help you find solutions to your cancer pain problems, either through carefully-prescribed painkillers that won’t interfere with your treatment, or through integrative medicine – a relatively new technique in patient care that aims to tackle problems with a patient’s health through a combination of alternative treatments and traditional Western treatments, seeking to find a solution to the pain, rather than masking it.
Also known as a “holistic approach”, a pain specialist may introduce you to methods such as swimming and strength training to strengthen the muscles surrounding a tumor and prevent cramping, acupuncture to relieve nerve pain, stretching to relieve soreness, nutrition to improve your overall health, and other activities to stimulate your body’s natural painkiller responses.
Deal with Joint Pain
Joint pain is a common complaint, especially with an advancing age. The joints are particularly vulnerable due to their role in storing excess uric acid, and their constant usage. While all joints deteriorate with time, some do faster than others. This can be due to injury, larger amounts of stress, or inflammation from an aging immune system or poor health.
While joint pain might seem like a natural part of aging, it does not have to become an excruciating fact of life. A pain management specialist can help you address the causes of your own joint pain. They also formulate a plan to reduce and control swelling and inflammation, and help you put yourself back on track for a life without constant pain and discomfort.
Over-the-counter painkillers and nonsteroidal anti-inflammatory medication, such as aspirin and the newer Celebrex, can reduce swelling and inflammation acutely. However, these are not a good long-term solution.
Eliminating certain foods and introducing more anti-inflammatory foods into your life can help your body address swelling and inflammation in the joints, as well as general pain. Ginger, for example, is a cheap and efficient supplemental food. It’s also easy to implement into your diet through freshly-made teas, low-sugar or sugar-free desserts, and Asian cuisine.
Regular exercise to warm up the muscles and stretch the ligaments greatly helps the body cope with joint pain. Exercise even goes so far as to massively reduce the pain and stiffness introduced by arthritis. However, without proper supervision and a careful exercise plan, or excessive stress, working out can make certain pain much worse. A pain management specialist can help you create an exercise and diet plan to help you deal with your pain. They focus on doing this without breaking the bank or messing up your work schedule.
Address Pregnancy Pains
Pregnancy is not an easy period in a woman’s life. Aside from the uncomfortable experience of obstetric pain and labor-related discomfort, the weight and size of a growing fetus can contribute to considerable back pain. It can also lead to neuropathic pain from pinched or pressured nerves, and cramping or swollen muscles and joints.
Pain management during pregnancy is more sensitive than in most other cases. This is because pain management specialists have a limited toolset to work with to avoid causing damage to the child. Certain painkillers are out of question. Similarly, to ensure the child’s safety, exercise if often limited. Dietary recommendations are completely different since mothers must avoid certain supplements to ensure a healthy birth.
However, in certain cases, a comprehensive approach to intolerable chronic pain may require the use of medication that is not 100% safe. Studies have concluded that a humane approach requires a specialist to consider both the fetus and the mother. This is because untreated chronic pain may lead to hypertension, anxiety or depression after and before birth. Chronic pain can endanger both the mother and the child.
Because of this, pain management during pregnancy is incredibly complicated. It requires the use of non-dangerous, non-opioid analgesics, and the consideration of opioid analgesics such as codeine and meperidine.
Pain management requires more than a cookie-cutter approach. Like any other medical discipline, a patient must be thoroughly and efficiently examined to determine what’s gone wrong. After examining what is wrong, we can then determine how to help fix it.
Pain management specialists take the long-term into consideration, battling chronic pain with a focus on a patient’s longevity, the potential side-effects or harmful consequences of certain therapies or medication, and much more. Be sure to choose the very best when looking for help regarding pain management.
Living With Chronic Pain and Finding Gratitude

Chronic pain is one of the most misunderstood conditions a human being can struggle with, because it is so strange and unusual. Because of this, living with chronic pain can be extremely difficult. Most people understand pain as a sharp sensation, a temporary warning that accompanies some sort of immediate threat/danger, or injury.
If you cut yourself, your brain signals you to pay attention to the cut, treat it, and keep it away from any physical contact. Your skin becomes hyper-sensitive, and you prioritize getting away from that feeling of hurt.
Chronic pain is different. It doesn’t go away. It doesn’t have a good reason to exist in the first place. It’s just pain, coming and going, always there, making life miserable for anyone who suffers from it. But because it’s so difficult to comprehend, people often can’t help but say things like “it can’t be so bad” or “you’re just exaggerating”.
This makes living with chronic pain especially difficult. Not only do you have to deal with the pain, but with the stigma of not being able to do many “normal” things. However, even with these challenges, life is still worth it. And here’s how you can make it work.
What You Need to Know About Living With Chronic Pain
Firstly: you’re not alone. While chronic pain isn’t extremely prevalent, we do live in an increasingly small world, and there are countless places both locally and virtually where America’s chronic pain population can come together for support, motivation, and leisure.
It’s not just America. The Internet lets you see what it’s like living with chronic pain in other countries. It lets you see how different people from completely diverse backgrounds deal with many of the same issues, and still manage to find a little joy in life. There’s a whole community out there, ready to share with you what it’s like to not just struggle with chronic pain, but manage it. By interacting with others working with chronic pain management, you can do the same.
When living with chronic pain, it’s important to remember: you still have friends and family. People who care for you, are patient through the hard days, and make it possible for you to live a “normal” life with a clean home, healthy food and loving company.
No matter how bad some days get, life is still life. It goes on, and better days are always on the horizon. And even if you can’t do some of the things that you used to do, life can still make you smile, laugh, and love.
What Others Need to Know
The most important thing others should know about living with chronic pain is this: it’s seriously hard being in pain all the time.
It can cut into your appetite and keep you from moving, causing muscle atrophy, lowering your self-esteem and making you feel even more miserable. And when you just want to lie down and sleep, some nights the pain is so bad that you can’t even drift off in peace. Pain keeps you from enjoying time with your family, and time to yourself.
Thankfully, life isn’t all pain in most cases. Some days are good, good enough to allow walking. Some days, however, the pain is so much that you can’t even sit down, let alone stand or go for a stroll. Misunderstanding a good day for a sign of significant improvement just makes someone living with chronic pain feel worse about themselves.
Finally; they’re still human beings. They get angry. They can be miserable. It’s important to be patient and empathic.
The Role that Gratitude Plays When Living With Chronic Pain
When living with chronic pain, it’s important to appreciate the good things in life, because otherwise, the pain wins. It will swallow you whole and leave nothing but a shell of your former self. But you’re more than that. Just because you’re in pain doesn’t mean you’re no longer you – you’re still you, you’re still human, and you still have the power in your mind to mean something to others, have a purpose and achieve personal greatness.
The first step to realizing that, however, lies in being happy and grateful for the gifts of life that you can still enjoy to this day.
It’s true that life will never be easy living with chronic pain, but it can be great. Even with the pain, life is worth living if you have the power to feel grateful for the good days, and the happy memories. And with a little imagination, there is so much left for you to do despite the pain – far more than you could ever accomplish in a single lifetime.
Diseases like fibromyalgia and chronic fatigue don’t have to be a death sentence – they may be challenging, and hard to deal with, but with the help of your loved ones and your own sheer will, you can still live a fulfilling and happy life. Through different techniques for pain management, living with chronic pain can be easier.
Pain Assessment: How Bad is Your Pain?

Science argues that pain is a subjective experience. Some pain experts agree that part of feeling the pain is how your brain is interpreting it. Fortunately, whether it’s all in your head or not, there are pain assessment tools to determine how bad your pain is. Here are different types of assessment tools to help you accurately portray your pain levels to professionals.
The 10-Point Pain Scale
Many doctors use a 10-point pain assessment scale, with 0 being no pain and 10 being an excruciating, debilitating pain. Yet, even this can be highly subjective. Two people with the same degree of pain might assess their pain differently – one at a level 5 and the other at a level 7 – depending upon their relative experiences. Because of this, there are other pain assessment tools to consider as well.
Other Pain Assessment Tools
To help people be more specific about their pain assessment and to determine just how severe pain might be, the LOCATES scale can help draw more information about the type of pain a person is experiencing. The LOCATES scale was developed by the American Pain Foundation (no longer in operation), and it continues to be a reliable tool to facilitate communication between health professionals and their patients.
The LOCATES pain assessment scale asks for the following information:
L – Location of the pain: Where is your pain and does it travels to other parts of your body?
O – Other associated symptoms: Do you have nausea, numbness, or weakness with your pain?
C – Character of the pain: Is it throbbing, sharp, dull, or burning?
A – Aggravating and alleviating factors: What makes the pain better or worse?
T – Timing of the pain: How long does the pain last? Is it constant or intermittent?
E – Environment: Where do you experience the pain most often – for example, while working or at home?
S – Severity of the pain: How would you rate your pain on a 0-to-10 pain scale, from no pain to worst ever?
While the above tool does use a 10-point pain assessment scale, it also invites more details about the level, type, factors, and symptoms of the pain. Those experiencing pain may want to share their answers to the above questions with their healthcare provider. Conveying these answers to your doctor can help you both create a pain management plan.
The Process of Pain
The process of pain is actually somewhat complex. It begins with the body’s vast neural network and millions of tiny sensors that exist throughout the body. Pain can be experienced when a nerve in the body has been triggered. However, there must be a certain amount of stimulus for pain to trigger.
For example, let’s say you have a bowling ball resting on your big toe. Yes, it’s heavy and it’s likely uncomfortable, but the weight of the ball isn’t enough to stimulate pain. Yet, if a bowling ball were to drop on your big toe from a few inches up, the falling weight of the bowling ball would stimulate a great deal of sensors, activating a nerve. This nerve, in turn, will produce a signal that travels up the spine to the brain. Interestingly, a person hasn’t yet experienced any pain. It is not until the signal from the nerve reaches the brain where it is processed and then you may have a response to what just happened.
Experiencing Pain
Your response and experience of the pain is based upon:
- the information taken in from your senses
- information from past experiences that may have been similar
- your current mood
- level of stress at the time
- perception of the situation
All of this is factored into the equation, without you consciously being aware that the brain is processing all this information, and then you decide the degree to which you experience pain. Within milliseconds, the brain decides whether a response to the situation is necessary. In this case, a person might jerk their foot back, scream, sit down, or do another activity in response to what they are experiencing.
However, the brain might not register the pain at all. Take for instance someone who has a severe case of diabetes and who experiences nerve damage in their foot. A bowling ball may fall on their toe or they may step on a nail and not feel the pain at all. This happens because the nerve that would normally send the signal of pain up to the brain has been impaired.
How to Respond to Pain
Depending upon your pain assessment; the type, location, and severity of your pain, you may want to respond to pain appropriately. There are some important tips to remember when it comes to experiencing pain in the body:
- Don’t ignore pain. Pain that is unknown to you or the result of an injury or disease should be assessed by a healthcare provider.
- Avoid painful movement. While your pain is still acute, it may be best to refrain from movement that causes more harm.
- Keep a pain diary. If you continue to experience pain and you’ve already consulted with a doctor or other healthcare provider, keep track of when, where, and how you experience pain. This can help build awareness around your pain.
- Take care of yourself. Be sure to eat well, get good sleep, and exercise (if you can) in order to keep your body healthy. This can help minimize your experience of pain.
- Drink plenty of water. It’s also important to keep the body hydrated.
- Be curious about your pain. Sometimes pain is not what you think. For example, pain in your neck and shoulders may have more to do with a misalignment in your hip. Again, talk to a healthcare professional if you suspect pain may be linked to something else.
- Reduce the amount of stress in your life. Experiencing pain is already a stressful experience. To help keep stress levels low, eliminate other sources of stress in your life as best you can.
These are general suggestions to keep the body healthy while facing pain. There are a great number of causes of pain. So, be sure to consult your doctor or a healthcare professional for suggestions to assist you in your unique situation.
When you do talk to a pain doctor or a healthcare professional, be sure to use the LOCATES pain assessment tool (or another pain assessment scale) to provide the most detail about your experience of pain. This can assist with getting the right treatment and professional support.
Natural Pain Relievers and Anti-Inflammatories
Medication is not the only reliable way to relieve pain – and for many, long-term medication is not a very suitable way to relieve chronic pain, which can plague a person for years. While most of our pharmaceutical options rely on natural extracts anyway, there are specific benefits towards applying some of nature’s own natural pain relievers in their original form.
But to understand why the common advice of ginger, turmeric, and less known relievers such as cloves all work in the face of specific forms of pain, it’s important to cover the basics of chronic pain, and the common cofactor of physical inflammation in the human body.
Chronic Pain and Inflammation
Chronic pain is a condition wherein a person experiences the sensation of pain regularly for over twelve weeks. Pain experienced regularly within that period is most likely acute. This pain is a derivative of a specific wound or injury, and fading as per the body’s own natural healing.
But our bodies are far from perfect. Through a range of possibilities from nerve damage, to inflammation and psychological illness, the body can achieve a state of chronic pain. Permanently treating chronic pain isn’t always possible, depending on its origins. The primary focus for medicine and treatment is to first look towards effective, long-term relief, while trying to identify the cause and an ultimate solution.
That’s where the science of pain management is most significant. Chronic pain management is a very broad school of knowledge, but its roots lie in understanding how pain travels from the body to the brain and back, and how specific pain relievers can block or counteract the signals.
Types of Inflammation
Inflammation isn’t always directly related to chronic pain, but it’s most definitely a part of pain in general. Inflammation is most often seen in the form of arthritis, a widespread joint inflammation that causes chronic joint pain. It occurs when an injury, infection, or other type of physical irritation or sickness causes the body to heat up and increase the overall sensitivity of a specific part. An inflammation around a wound is typically a sign of infection, for example. As the body’s immune system is working hard to fight foreign bacteria through white blood cells, the increased activity results in heating up the wound, and making it more sensitive to discourage any contact.
If you cut yourself or break a bone, then any attempts to touch the injured area will result in extreme discomfort. Even with a mild or soft touch will hurt, to prevent further damage – the same thing happens in an inflammation.
The problem when inflammation is tied to chronic pain, is that the inflammation may not go away. Aside from the obvious drawback of near-constant pain, an inflammation anywhere in the body will weaken you tremendously, and sap your energy.
In many cases of chronic pain, fighting not just the pain but specifically fighting to lower any internal inflammation often works to further decrease pain. When it comes to natural pain relievers and anti-inflammation, the options for application remain the same: external, and internal.
Topical Natural Pain Relievers
Pain relief often comes in the form of creams and ointments. There are several naturally-derived ointments that are perfect for quick pain-relief, especially in cases of back pain and arthritis. A few examples include:
Among these three Cs, camphor is most often found in ointments and paired with menthol. Capsaicin is the active element in hot peppers. It’s unique nerve interaction causes it to become an effective numbing agent when used right. Comfrey shouldn’t be ingested, but is an active ingredient in a topical cream it is effective for pain management.
Pain Relief Through the Diet
Let food by thy medicine – and despite thousands of years of progress in the sciences, Hippocrates early wisdom still holds true. While a good diet won’t exactly patch up a knife wound or splint a broken arm, most preventative diseases can be greatly diminished and even avoided entirely through healthy lifestyle choices. Genetics, environmental factors such as pollution and even psychological factors can still skew the outcome against you. However, healthy food can keep you fit – or in this case, relieve a lot of pain.
Foods That Lower Inflammation
There are quite a few ways to relieve pain and lower inflammation through food, including:
- Willow bark tea
- Turmeric
- Omega-3 and omega-6 foods
- Other fats
- Leafy greens
- Berries and citrus fruits
Willow bark and turmeric are ancient natural pain relievers, and modern-day aspirin specifically derives from willows. Omega-3 fats are present in seed oils and most plants, while omega-6 fats are in seafood. The trick is doing your best to maintain a low ratio of the two. Research shows that doing this greatly decreases inflammation – rather than just eat more fish, cut down on all seed oils.
Healthy fats come in many shapes and forms. Avocados, coconut, lean meat, fish, and olives are great sources of fat, while seed-derived oils, lard and margarine aren’t. A healthy balance of green vegetables and various fruits also decreases inflammation. Although the jury is still out on exactly why this is, as antioxidants may not be as important as we’ve thought.
Foods to Avoid
Sometimes, what you don’t eat matters as well. There are specific foods to avoid when you’d like to decrease your pain and inflammation, and stay healthier in general. These include:
- Refined sugars/carbs (including white bread and pasta)
- Canned and/or processed meats
- Trans fats, margarine, shortening
- Fried foods (excessive seed oils)
Acupuncture
Other natural pain relievers to consider are a bit more exotic, but shows a kind of promise that is not to be ignored. Acupuncture, an ancient medical practice, is surprisingly effective in many cases of chronic pain although we can’t really say why. The answer might lie in future research, or in the simple placebo effect. Either way, it’s a type of therapy that, considering the odds, would be well worth a shot.
It’s possible that just like acupuncture, some of these topical or natural pain relievers won’t function well. We humans do have a shared biology, but we’re still individually unique – certain factors from genetics to diet and medical history may mean that some tools are far less effective than others. It all depends on the origin and kind of chronic pain being experienced, as well. In terms of anti-inflammation, however, it’s more straightforward and generally applicable. Diet is an effective way of controlling your body’s inflammation, and with time, a good diet and regular exercise can help you lead an enjoyable and fulfilling life even with the diagnosis of chronic pain.
How Fibromyalgia Pain Relates to Other Pain Conditions

Pain is not something we’re particularly inclined to like, as its intended function is to be something we actively avoid and work against. But there is such a thing as useful pain. Pain that teaches us valuable lessons in life, like avoiding fire and minding our step.
But there is some pain that has absolutely no use, and no meaning. Medically, that pain is part of a series of disorders – conditions like fibromyalgia, which plagues roughly 5 million American adults. These people must live with chronic fatigue, constant soreness, and the combined blight of widespread pain and a heightened awareness towards it. We don’t know what causes this disease. We don’t know what cures it. But we have learned to help people deal with it, and live meaningful lives.
To properly understand this affliction, it’s important to first tackle how pain itself works – and why fibromyalgia is a massive physical ailment with system-wide consequences. We must first understand how fibromyalgia pain relates to other pain conditions before we can understand how to relieve this pain.
What It Means To Be In Pain
The human body processes stimuli and undergoes a series of brain functions to classify the experience and determine how to react to it. When you experience something pleasant, like a hug from someone you care about, your body interprets it accordingly by releasing certain neurochemicals that make us “feel” a certain way. It gets more complicated than that when you enter the realm of psychology and personality, but from a neurological perspective, it’s a mechanical process.
When the body experiences harmful stimuli, the brain receives a different kind of signal, one that lets it know that there’s a potential danger nearby. Before you can even think about contextualizing the pain, the body and your brain react instantly with irritation, or fear, or a reflexive action such as backing away or flinching. In some cases, pain activates our inner fight or flight response, and the release of adrenaline, epinephrine, and norepinephrine.
From an evolutionary standpoint, certain things make us feel pain so we can learn to avoid them. This ranges from something as obviously dangerous and malicious as a powerful smack to the head to something as unexpected as social rejection. When we feel pain, our initial reaction is not to like it, and then we can act on that info. Simple, and effective.
It gets more complicated on a person-to-person basis, though. Pain is generally objective, but the individual experience is subjective. What you consider painful will be different from what your spouse may consider painful, and tolerance levels for pain change from person to person. We also experience pain differently depending on our mood and emotional stability, our psychological state, our expectations of incoming pain, and quite significantly, the various experiences we might’ve had with pain in the past. Generally-speaking, pain can be split between “physical” pain (nociceptive), generated by a cut, a bruise, a broken bone or another injury; neuropathic pain, which isn’t generated by damage to the body but instead direct interaction with the nerves (nerve damage, spinal cord damage, pain disorders); and psychogenic pain, which is a feeling applied to existing pain by deep psychological troubles and worsening expectations.
While pain is meant to be our cautionary friend in most cases, there are times when it’s not quite so effective at doing its job of keeping us safe and healthy. In this case, the body and pain have a long-term toxic relationship, rather than the ideal distant acquaintance.
On Fibromyalgia Pain
Fibromyalgia pain is a full-body affliction that primarily affects your muscles and connective tissue, and the main symptom reported by those suffering from the condition is widespread chronic (more than 12 weeks) pain. In addition, fibromyalgia pain comes with weakness, nerve pain, muscle spasms and twitching, sleep disturbance and fatigue, and a heightened reaction to physical contact and touch (more pain).
While it affects the muscles and connective tissue, fibromyalgia is a disease of the brain. No one knows concretely what causes it other than an individual and subjective combination of genetics and environmental (lifestyle) factors, and there is no direct cure for the disease either. What basically happens when it develops is that your nervous system malfunctions and begins to sense pain when really there shouldn’t be any, and any painful stimuli are made much more powerfully repellent.
This is a neurological disorder, rather than a psychiatric one, and it’s a disorder with such capacity for widespread emotional damage that dealing with it can be an absolute nightmare.
Fibromyalgia is at its core a problem with pain reception, but it’s also very often part of a comorbidity: the combination of different related afflictions. For example, the chronic pain from fibromyalgia can cause chronic headaches, myofascial pain syndrome (constant muscle soreness), and other forms of rheumatoid pain including arthritis in the joints. Like a multiplier, any acute pain or syndrome you’re suffering from is felt more intensely under fibromyalgia pain. A few common comorbidities for fibromyalgia include:
- Chronic fatigue
- Inflammatory bowel disease
- Interstitial cystitis
- Temporomandibular joint dysfunction
- Arthritis
These are forms of inflammation physical irritation, heightening the body’s sense of pain. This is factored in by the body on top of any subjective thoughts, attitudes and experiences you may already have regarding pain – the result is a chronic condition that can affect you either in a localized fashion (severe hip or shoulder pain, or a specific muscle soreness) or in a general fashion.
Dulling the Hurt
As mentioned previously, there is no direct cure for fibromyalgia pain currently available, but there are several non-steroidal and corticosteroid painkillers available per prescription and over-the-counter to combat the chronic pain brought along by fibromyalgia.
Like so many other pain conditions, the danger with this one is that constant pain is bound to complicate the emotional and psychiatric health of many patients, which only further deepens the possible pain and encourages the use of maladaptive coping strategies like addiction and reckless behavior to take the edge off.
Aside from medication, what seems to work best is a lifestyle change. The inflammatory symptoms and increased pain can be managed properly by following a strictly healthy living regimen, including:
- A diet of fresh food, especially nutrient-rich vegetables and fresh seafood.
- Regular albeit moderate exercise, to improve the body’s neurochemical balance and stave off muscle weakness.
- Consistent and long sleep, to ensure as much rest as possible.
- Movement therapies like tai chi and yoga to raise awareness and body control, useful for mentally dulling out the pain.
Every case is different, and every proposed pain management plan must be catered to the patient’s means, symptoms, and total diagnosis. While fibromyalgia isn’t curable, it is highly treatable and manageable, and a lot of people live with it without medication, relying simply on physical and psychological therapy to overcome the pain. Some rely on alternative treatments like acupuncture and cupping therapy. Like chronic pain in general, it’s a long and tough road – but it’s most definitely a life worth living.
When An Injury Turns Into Chronic Pain

Research has shown that pain affects over one hundred million people, as reported by primary care physicians. Addressing pain can be simple for some and extensive for others, depending on the type of injury. You may have a simple fix, like a broken finger that gets a splint and is healed with a few months. Or you may have a pain that can’t be found through any scans, tests or examinations and lasts for years.
Sometimes it can be both. What you think is going to be a quick fix and starts out as an injury turns into chronic pain and a long treatment period. There are many different types of injuries and all of them have the potential to lead to chronic pain if not managed correctly.
Injuries
Acute pain is the pain typically associated with an injury. It is our body’s way of yelling,
“Hey you, there is a problem here. Fix it soon or else.”
Injury is defined as damage, harm or loss, usually from an outside source. There are many types of injuries, just ask any personal injury attorney. I bet you have experienced at least one in your lifetime, if not more. Have you ever sprained your ankle, cut yourself with a knife, or missed the nail and hit your thumb when using a hammer? Then you have had an injury. Ever been in a fender bender and for the two weeks following had a stiff neck? Then you have had an injury.
There are sports related injuries such as pulled muscles, dislocations and shin splints. There are work related injuries that include machine related or toxic substance exposure. There are also construction related injuries, pet related injuries, car related injuries, playground injuries, the list goes on and on. Basically, if you are living your life, you are susceptible to an injury. But that is no reason to stop living. Not at all. Injuries are very fixable and can heal within a short amount of time.
The medical world defines injuries in more specific terms, like soft tissue, bone, skin and by the body part that is injured. Injuries typically last less than 12 weeks. When an injury turns into chronic pain, it can lead to a long treatment period.
How Pain Becomes Chronic
If you are struggling with an injury in which the pain just won’t go away, then you may be experiencing chronic pain. Pain becomes chronic when it does not leave after three or four months. Your three or four months may be feeling more like three or four years. Persistent pain puts a strain on all parts of our lives and can slow us down or stop us altogether.
One study found that your body’s cells can keep a memory of the injury. Even though the injury is healed and gone, the memory of that pain stays with you in the nerves located around the injury. This happens because your nervous system remains sensitive long after the actual injury has healed.
Chronic pain tends to show up more in older adults, but it does not discriminate. It can affect people of all ages. People who have had surgeries, injuries and are obese tend to experience chronic pain more than others. So, just what is chronic pain?
Chronic Pain
Chronic pain is the type of pain that loves to hang around and make your body its home for twelve weeks or more. It’s like that cousin who came for a week’s vacation and is still living with you three months later. It does not go away and it can interfere with your daily routine.
Chronic pain can appear in many different forms. A few examples are headaches, fibromyalgia, back pain, diabetes and arthritis. Sometimes pain can affect you with no diagnosable reason. Over 30 million people are suffering from chronic pain in the United States alone.
The good news, you can get help in managing your pain.
The Importance of Chronic Pain Management
Chronic pain is not something that will just magically disappear and it is not something you should try and manage on your own. A pain management physician is the person you need to help you overcome your pain related issues. He or she has a medical degree and specialized training in pain. They are experts on all things pain. Their goal is to treat your symptoms so you can live a functioning life.
A pain management physician will most likely recommend a variety of treatments and therapies to help you cope with your pain. This is because it is important to treat all areas of your body that will most likely be affected by your pain. The more experts helping you, the better. They will be your own special treatment team and all of them will have the same goal, easing your pain as best they can.
Build Your Team
Your team should consist of a variety of healthcare professionals, friends and family members who truly want to see you succeed in the management of your pain. You do not want people in your life who just want to give you pain pills and let you sleep all day.
A pain management physician is one who can prescribe appropriate medications and monitor you closely to make sure the medicines are working and if not, help you find other medical treatments. They can also examine you on a regular basis and measure for improvements.
A psychologist should be on your team. They can help you work through the mental health issues you may encounter when it comes to pain. They can also help you treat your depression, anxiety or stress that is related to the pain.
A physiatrist and an anesthesiologist are also good team members. A physiatrist has an education in physical medicine and rehabilitation and can treat problems with the brain, nerves, bones, muscles, tendons and more.
A physical therapist can teach you specific exercises and movements that will help you ease pain where it is persistent.
Alternative therapies can also be beneficial to help ease some of your pain. Therapies such as acupuncture, yoga, massages and herbal remedies. There are many holistic practitioners who can help you focus on the mind, spirit, body connection to ease your pain.
Your friends and family should be on your team to help you stay positive, get some exercise, eat healthy and meet other needs your doctors can’t. They are not in your life to enable you, however, only to assist you in completing your own tasks.
Just because you have chronic pain does not mean you can’t have a happy life. There are many resources to assist you in managing your pain. You are valuable, purposeful and worth the effort!